Worldwide, more than 300,000 babies are born with sickle cell disease each year. It is the most common inherited blood disorder in the United States, affecting around 100,000 people nationwide. June 19th has been designated as World Sickle Cell Day with the goal of increasing knowledge and understanding of sickle cell disease as well as raising awareness of the challenges experienced by patients, their families, and their caregivers.
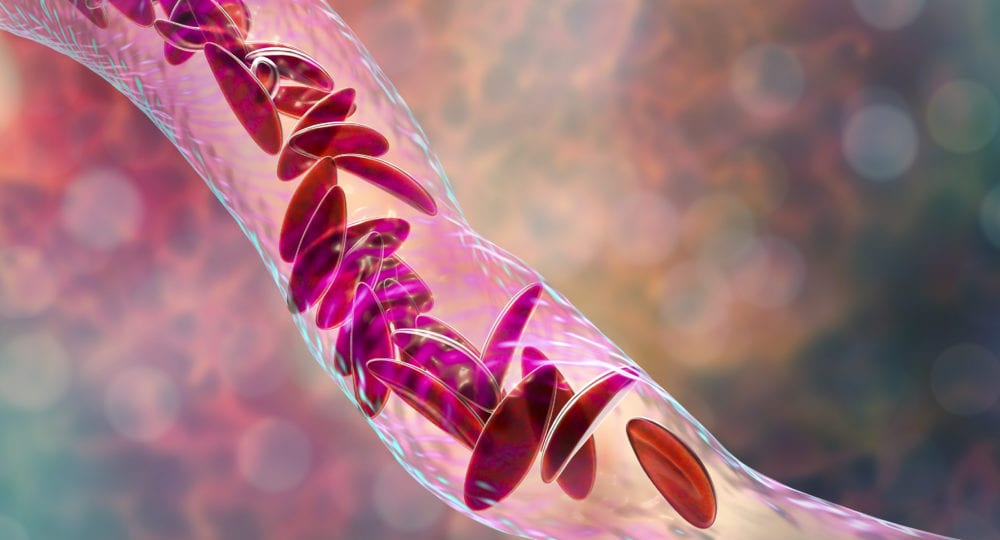
Healthy red blood cells are round, and they travel through blood vessels to carry oxygen to all parts of the body. Sickle cell disease (SCD) is a group of inherited red blood cell disorders. In SCD, the red blood cells become hard and sticky and have the shape of a C-sharped farm tool called a “sickle.” The sickle cells die early, which causes a constant shortage of red blood cells. They can also get stuck in blood vessels as they travel, blocking the flow of blood, causing pain and other serious complications.
SCD is a genetic condition that is present at birth. It requires that a person inherit a sickle cell gene from each of their parents.
Sickle cell trait (SCT) occurs in people who inherit a sickle cell gene from one parent and a normal gene from the other. These people do not usually have any symptoms of SCD, but they can pass it to their children. If two partners both have the trait, they have a 1 out of 4 chance of having a child with SCD.
It is thought that SCD occurs more often in people from parts of the world where malaria is or was common because people with sickle cell trait are less likely to have severe forms of malaria. This is why it is more common in people of African heritage. In black or African American babies, about 1 out of every 13 is born with SCT, and 1 out of every 365 is born with SCD.
SCD is diagnosed with a blood test. It can be diagnosed prenatally but is most often found at birth with a newborn screening test. Early diagnosis and treatment are important to prevent and reduce complications.
Health complications faced by those with SCD include:
- Pain episode or crisis- sickle cells don’t move easily through small blood vessels and can get stuck; this causes pain which can start suddenly, be mild to severe, and last for any length of time (hours to days)
- Anemia- decreased red blood cell count; this can cause tiredness, irritability, lightheadedness, increased heart rate, difficulty breathing, slow growth, and delayed puberty
- Infection- increased risk of getting a harmful infection (e.g. flu, meningitis, pneumonia, hepatitis) due to damage to the spleen which decreases its ability to filter bacteria from the blood
- Hand-foot syndrome- swelling in hands and feet, often with a fever, due to sickle cells blocking blood from flowing through the hands and feet
- Eye disease- restricted blood flow to the eyes can lead to long term vision problems
- Acute chest syndrome- blockage of blood flow to the lungs can cause chest pain, coughing, difficulty breathing, and fever and can be life-threatening
- Stroke- blockage of blood flow to the brain which can cause lifelong disabilities and learning problems
- Other blood clots – especially in a deep vein or lung, can cause serious illness, disability or even death
- Damage to organs (e.g. liver, heart, kidneys), tissues or bones because of reduced blood flow to those areas
- Malnutrition, growth retardation, delayed puberty, and infertility in males
As knowledge and research about SCD continue to grow, so does the outlook for those with the disease. The average life expectancy of a person with SCD, which was less than 20 years of age in the 1970s, had risen to 38-42 years in 2005. Pneumonia is a leading cause of death in infants and young children with SCD, and reduction in mortality rates coincided with the introduction of a vaccine protecting against invasive pneumococcal disease in 2000.
Early and ongoing medical care can minimize complications and help those with the disorder lead full and active lives.
Preventative measures can help people with SCD reduce their complications:
- High fluid intake (8-10 glasses of water each day)
- Avoiding getting too hot, too cold, or too tired
- Infection prevention
- Vaccines are especially important
- Good hand hygiene
- Safe food prep
- Prescription antibiotic (often penicillin) taken daily until at least 5 years old
There is no single best treatment for people with SCD. Treatments can include:
- Blood transfusions
- Intravenous (IV) fluids
- Medications to help with pain
- Hydroxyurea- a medication for adults with severe SCD that can reduce pain, the recurrence of acute chest syndrome, and may reduce the need for blood transfusions and hospitalizations
The only cure for SCD is a bone marrow or stem cell transplant. Bone marrow is the tissue inside of bones where blood cells are made. A transplant involves taking healthy cells from a donor and putting them into someone with SCD. It can be risky and have serious side effects including death, so it is only used in children with severe cases of SCD who have minimal organ damage from the disease. For it to work, the bone marrow must be a close match and often comes from a sibling or other close relative.
Another treatment being studied is gene therapy. This involves removing affected stem cells from the patient’s bone marrow or blood and adding to it a therapeutic gene which is defective in people with SCD, then returning the cells to the patient. This is showing promising results in leading to the production of anti-sickling hemoglobin.
—
Resources:
Sickle Cell Disease Association of America
Image by Dr_Microbe on iStock